World Alzheimer’s Month is in October, which is an ideal time for us to shine a light on the disease. We are going to explore the different types of dementia and discuss how not all dementia is not related to Alzheimer’s disease.
Dementia vs Alzheimer’s
Dementia and Alzheimer’s disease are sometimes used interchangeably. But they aren’t the same thing. Alzheimer’s is a disease in which dementia is a major component. Dementia is a term that refers to a group of brain conditions that may affect a person’s ability to think, remember, or remember. Also, people with dementia may lose visual perception, language skills, and the ability to contain their emotions.
Even though dementia is common among older people, it is not considered a normal part of aging. It’s considered a health condition that needs to be monitored.
Symptoms of Dementia
The different types of dementia have their own unique set of symptoms. However, many patients with dementia will exhibit several of the symptoms below:
- Memory loss and distortion
- Loss of vocabulary
- Changes in mood and disposition
- Faulty reasoning
- Disorientation
- Trouble with comprehension
- Difficulty balancing
- Lack of self-care tendencies
- Change in appetite or eating habits
- Loss of social skills
- Disruptions in sleep-wake cycle
Types of Dementia
Alzheimer’s Disease
Alzheimer’s disease is the most common type of dementia. Between 60 and 80 percent of cases of dementia are caused by this disease, according to the Alzheimer’s Association. Early signs of Alzheimer’s disease include depression, forgetting names and recent events, and depressed mood. However, depression is not part of Alzheimer’s Disease. It’s a separate disorder that must be treated specifically. Occasionally, depressed older adults are misdiagnosed as having Alzheimer’s disease.
Alzheimer’s disease is characterized by brain cell death. As the disease progresses, people experience confusion and mood changes. They also have trouble speaking and walking.
Older adults are more likely to develop Alzheimer’s. About 5 percent of cases of Alzheimer’s are early-onset Alzheimer’s, occurring in people in their 40s or 50s.
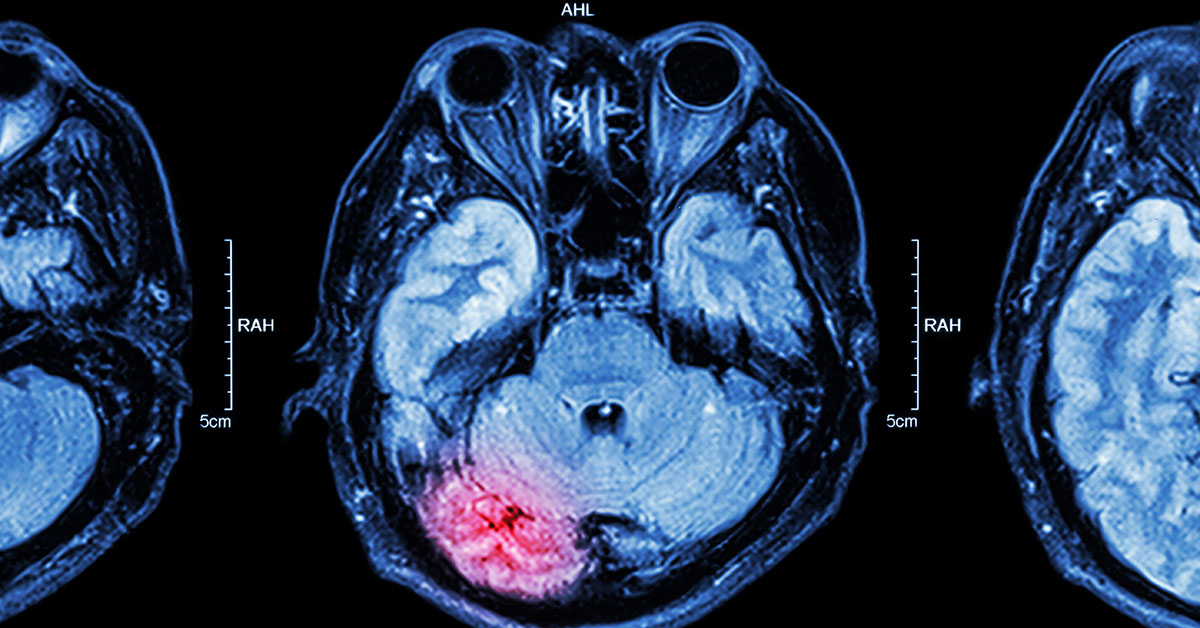
Vascular Dementia
The second most common type of dementia is vascular dementia. It’s caused by a lack of blood flow to the brain. Vascular dementia can happen as you age and can be related to atherosclerotic disease or stroke.
Symptoms of vascular dementia can appear slowly or suddenly, depending on what’s causing it. Confusion and disorientation are common early signs. Later on, people also have trouble completing tasks or concentrating for long periods of time.
Vascular dementia can cause vision problems and sometimes hallucinations as well.
Dementia with Lewy Bodies
Dementia with Lewy bodies, also known as Lewy body dementia, is caused by protein deposits in nerve cells. This interrupts chemical messages in the brain and causes memory loss and disorientation.
People with this type of dementia also experience visual hallucinations and have trouble falling asleep at night or fall asleep unexpectedly during the day. They also might faint or become lost or disoriented.
Dementia with Lewy bodies shares many symptoms with Parkinson’s and Alzheimer’s diseases. For example, many people develop trembling in their hands, have trouble walking, and feel weak.
Parkinson’s Disease
Many people with advanced Parkinson’s disease will develop dementia. Early signs of this type of dementia are problems with reasoning and judgment. For example, a person with Parkinson’s disease dementia might have trouble understanding visual information or remembering how to do simple daily tasks. They may even have confusing or frightening hallucinations.
This type of dementia can also cause a person to be irritable. Many people become depressed or paranoid as the disease progresses. Others have trouble speaking and might forget words or
Frontotemporal Dementia
Frontotemporal dementia is a name used to describe several types of dementia, all with one thing in common: They affect the front and side parts of the brain, which are the areas that control language and behavior. It’s also known as Pick’s disease.
Frontotemporal dementia affects people as young as 45 years old. Although scientists don’t know what causes it, it does run in families and people with it have mutations in certain genes, according to the Alzheimer’s Society.
This dementia causes loss of inhibitions and motivation, as well as compulsive behavior. It also causes people to have problems with speech, including forgetting the meaning of common words.
Creutzfeldt-Jakob Disease
Creutzfeldt-Jakob disease (CJD) is one of the rarest forms of dementia. Only 1 in 1 million people are diagnosed with it every year, according to the Alzheimer’s Association. CJD progresses very quickly, and people often die within a year of diagnosis.
Symptoms of CJD are similar to other forms of dementia. Some people experience agitation, while others suffer from depression. Confusion and loss of memory are also common. CJD affects the body as well, causing twitching and muscle stiffness.
Wernicke-Korsakoff Syndrome
Wernicke’s disease, or Wernicke’s encephalopathy, is a type of brain disorder that’s caused by a lack of vitamin B-1, leading to bleeding in the lower sections of the brain. Wernicke’s disease can cause physical symptoms like double vision and a loss of muscle coordination. At a certain point, the physical symptoms of untreated Wernicke’s disease tend to decrease, and the signs of Korsakoff syndrome start to appear.
Korsakoff syndrome is a memory disorder caused by advanced Wernicke’s disease. People with Korsakoff syndrome may have trouble:
- processing information
- learning new skills
- remembering things
The two conditions are linked and are usually grouped together as one condition, known as Wernicke-Korsakoff syndrome. It’s technically not a form of dementia. However, symptoms are similar to dementia, and it’s often classified with dementia.
Wernicke-Korsakoff Syndrome can be a result of malnutrition or chronic infections. However, the most common cause of this vitamin deficiency is alcoholism. Sometimes people with Wernicke-Korsakoff syndrome make up information to fill in the gaps in their memories without realizing what they’re doing.
Mixed Dementia
Mixed dementia refers to a situation where a person has more than one type of dementia. Mixed dementia is very common, and the most common combination is vascular dementia and Alzheimer’s. According to the Jersey Alzheimer’s Association, up to 45 percent of people with dementia have mixed dementia but don’t know it.
Mixed dementia can cause different symptoms in different people. Some people experience memory loss and disorientation first, while others have behavior and mood changes. Most people with mixed dementia will have difficulty speaking and walking as the disease progresses.
Normal Pressure Hydrocephalus
Normal pressure hydrocephalus (NPH) is a condition that causes a person to build up excess fluid in the brain’s ventricles. The ventricles are fluid-filled spaces designed to cushion a person’s brain and spinal cord. They rely on just the right amount of fluid to work properly. When the fluid builds up excessively, it places extra pressure on the brain. This can cause damage that leads to dementia symptoms.
According to Johns Hopkins Medicine, an estimated 5 percent of dementia cases are due to NPH.
Some of the potential causes of NPH include:
- injury
- bleeding
- infection
- brain tumor
- previous brain surgeries
However, sometimes doctors don’t know the cause of NPH. Symptoms include:
- poor balance
- forgetfulness
- changes in mood
- depression
- frequent falls
- loss of bowel or bladder control
Seeking treatment as early as possible can help a doctor intervene before additional brain damage occurs. Normal-pressure Hydrocephalus is one of the types of dementia that can sometimes be cured with surgery.
Huntington’s Disease
Huntington’s disease is a genetic condition that causes dementia. Two types exist– juvenile and adult-onset. The juvenile form is rarer and causes symptoms in childhood or adolescence. The adult form typically first causes symptoms in a person when they’re in their 30s or 40s. The condition causes a premature breakdown of the brain’s nerve cells, which can lead to dementia as well as impaired movement.
Symptoms associated with Huntington’s disease include impaired movements, such as jerking, difficulty walking, and trouble swallowing. Dementia symptoms include:
- difficulty focusing on tasks
- impulse control problems
- trouble speaking clearly
- difficult learning new things
Schedule an Appointment
Regional Neurological Associates has reopened with your safety in mind and we are seeing patients in-office. Our current office hours are: Monday – Friday from 9 am – 4 pm. If you have questions or concerns about your neurological health, call us at (718) 515-4347 to make an appointment. We are also pleased to announce that same-day appointments are now available.
We do ask that patients experiencing symptoms like fever, cough, or shortness of breath reschedule your appointment or schedule a telemedicine appointment. Please contact our office to change your in-person visit to a Telehealth visit (718) 515-4347. We thank you for your understanding and cooperation.