Peripheral neuropathy, or simply neuropathy, is a term used to describe a large number of conditions that are related to damage in the peripheral nervous system. The peripheral nervous system is the network of nerves that send information from the brain and spinal cord (the central nervous system) to the rest of the body.
Your peripheral nerves are responsible for how your body functions as well as how it reacts to outside stimuli. When there is damage to the peripheral nervous system, complications occur that interfere with everyday life. Neuropathy is not a single condition, but a blanket term that covers many different conditions with different causes. To understand more about this condition, it’s helpful to learn about its causes and the different types of peripheral neuropathy.
Causes of Neuropathy
Neuropathy can be genetic, meaning it is present from birth. Or it can be acquired, meaning it was caused after birth. Acquired neuropathy is the more common of the two. Acquired neuropathies may be symptomatic of another disorder or disease. They can also be idiopathic, meaning there is no known cause.
Acquired peripheral neuropathy that causes symptoms can be caused by a wide range of things including:
- Physical trauma or injury
- Diabetes
- Vascular disease
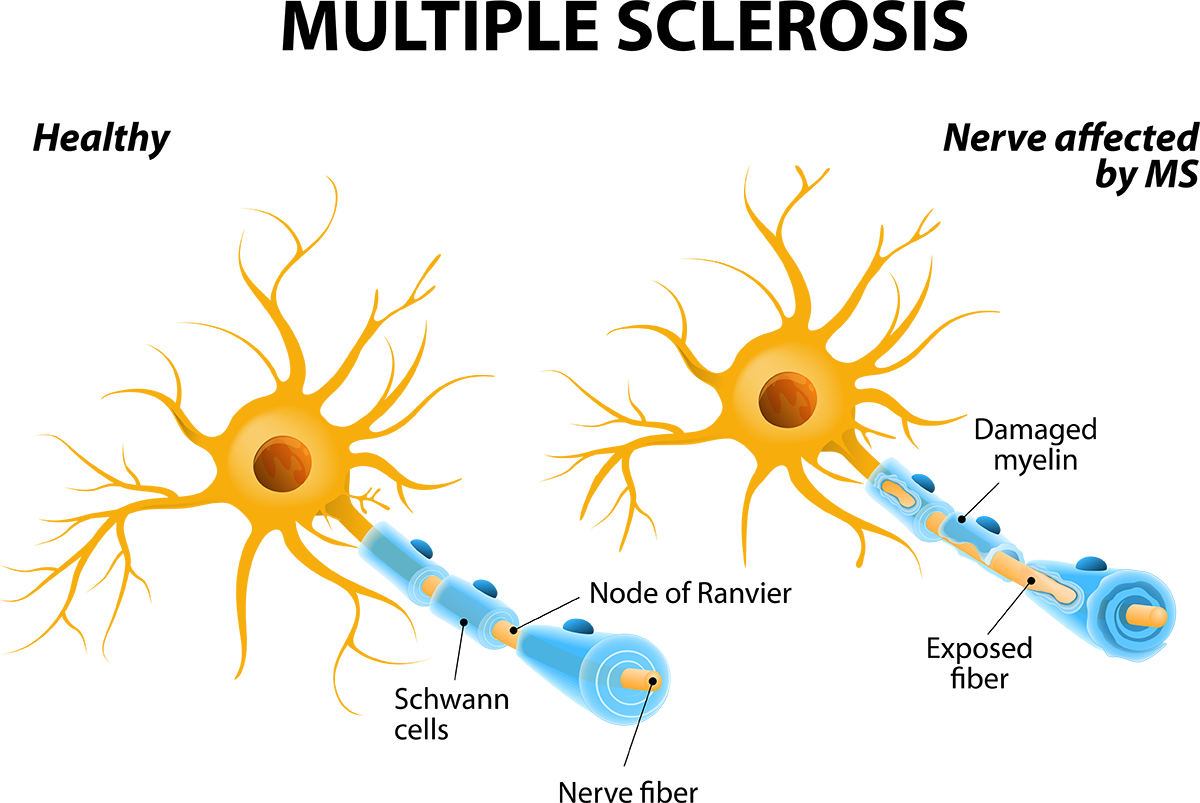
- Autoimmune diseases
- Systemic (body-wide) autoimmune diseases
- Autoimmune diseases that only attack nerves
- Nutritional imbalances
- Hormonal imbalances
- Cancer
- Chemotherapy drugs
- Infections
- Kidney and liver disorders
Types of Peripheral Neuropathy
The nerves in the human body can be broken down into three groups: sensory, motor, and autonomic. According to the National Institute of Neurological Disorders and Stroke, there are more than individual 100 types of peripheral neuropathy, but the can be categorized by which type of nerves are being affected:
1. Sensory
The sensory nerves are responsible for transmitting information about physical feelings and senses. For instance, when you feel either hot or cold, your sensory nerves are communicating those feelings between your brain and your body. Your sensory nerves are also responsible for detecting pain. Pain is actually a very useful sensation, as it protects people from injury (or further injury) by alerting them that something is wrong. When the sensory nerves are damaged, they do not transmit information correctly, causing a variety of physical symptoms and complications. Symptoms of sensory nerve damage include:
- Pain
- Worse at night for some individuals
- Severe pain may be caused by even the lightest touch. This is called allodynia.
- Ex: bed sheets lightly draped over the body causes pain
- Inability to feel vibrations or touch, especially in the hands
- Loss of reflexes
- Loss of sense of position
- Inability to coordinate complex movements
- Difficulty keeping balance with the eyes shut
- Inability to feel pain
- Inability to feel changes in temperature
2. Motor
Your motor nerves control all of your conscious movements. They are responsible for sending signals to all the muscles under conscious control. The motor nerves allow you to walk, talk, write and grasp things. Damage to the motor nerves interferes with voluntary movements. Symptoms of motor nerve damage include:
- Muscle weakness
- Painful cramps
- Uncontrolled muscle twitches
- Muscle shrinking
3. Autonomic
Your autonomic nerves control your organs and regulate all the actions that you do not consciously control. This includes breathing, heart function, digestion, and gland function. If these nerves are damaged, your body may lose the ability to regulate certain functions like blood pressure, responses to temperature, or even digest food. Symptoms of autonomic nerve damage include:
- Heat intolerance
- Excessive sweating
- Gastrointestinal symptoms
- Trouble eating or swallowed (only if nerves in the esophagus are affected)
- Inability to expand and contract small blood vessels to regulate blood pressure
Can Peripheral Neuropathy be Treated?
Treatments are available for neuropathy, but they depend on the type of neuropathy and its underlying cause. Controlling diabetes helps with diabetic neuropathy. Using immunosuppressive drugs can treat autoimmune disorders. If an underlying cause is successfully treated, then the neuropathy may resolve itself. This is because nerves can sometimes regenerate and regain function.
If neuropathy is idiopathic and has no discernable cause, that makes it more difficult to treat. Lifestyle changes can improve symptoms of peripheral neuropathy, whether the cause is known or not. Not smoking, maintaining a healthy weight, staying active, and eating a balanced diet can all contribute to improvement in neuropathy symptoms.
—
Regional Neurological Associates is home to board-certified neurologists who have expertise in treating a range of neurologic conditions, including neuropathy, headaches, epilepsy, MS, dementia, and stroke. If you have concerns about neurological disorders like peripheral neuropathy, call (718) 515-4347 to make an appointment.